Why Dual Diagnosis Often Goes Undiagnosed
When we think of addiction, we often picture the substance first: the alcohol bottle, the pills, the rolled-up note. What we don’t always see is what’s underneath: the anxiety that’s been ticking for years, the childhood trauma nobody noticed, the slow descent into depression masked by a social smile. That’s where dual diagnosis lives in the overlap between substance abuse and mental health disorders. And tragically, it’s also where many fall through the cracks.
So why does something this prevalent often go undetected?
Let’s break it down.
What Exactly Is Dual Diagnosis?
Dual diagnosis refers to the coexistence of a mental health disorder and a substance use disorder in the same individual. Think depression and alcohol abuse. Schizophrenia and methamphetamine use, anxiety and benzodiazepine dependence.
These aren't isolated conditions that randomly coexist. They interact with each other, feed off each other. One can exacerbate the other in ways that blur the clinical picture and confuse treatment providers who don’t specialise in both.
That’s why dual diagnosis rehab is its ecosystem — one that requires integrated, not siloed, care.
The Visibility Problem
Here’s the thing: most people don’t walk into treatment saying, “Hi, I have a co-occurring disorder.” They come in because something hurts. They can’t stop drinking. They’ve lost jobs, partners, and routines. They’re depressed, anxious, maybe hearing things, maybe paranoid. And often, they’ve been told they’re “just addicts.”
This is where the diagnostic failure happens.
When substance abuse is the loudest symptom, it overshadows the quiet ones. Therapists might chalk up hallucinations to meth-induced psychosis and miss the schizophrenia . Depression may be dismissed as a byproduct of withdrawal, rather than a pre-existing condition. The result? People get partial treatment for a whole problem.
Why This Happens So Often
1. Lack of Training Among Providers
Not all rehab staff are trained to identify or manage psychiatric illness. Many dual diagnosis treatment centres market themselves as such, but lack full-time psychiatrists or trauma-informed therapists. Without this, complex cases go unrecognised or are treated like simple dependency.
2. The Shame Barrier
Clients themselves might hide their mental health symptoms due to stigma. Imagine being in withdrawal and also telling someone you hear voices. The fear of being labelled “crazy” keeps many silent.
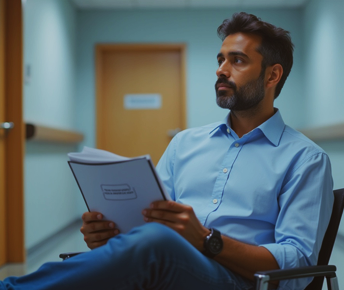
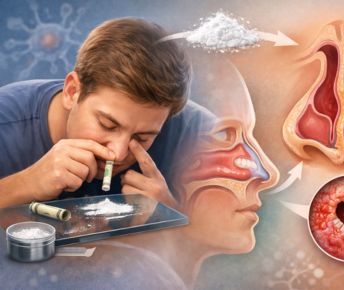
3. The Diagnostic Fog of Addiction
Substances blur the clinical picture. Cocaine can mimic mania. Alcohol withdrawal can resemble anxiety—Benzodiazepine cloud memory. Diagnosing a mental illness during active substance use is like trying to measure the depth of a lake during a storm.
4. Treatment Silos
Historically, mental health and addiction treatment were separate worlds. You went to one centre for therapy and another for detox. But co-occurring disorders demand a dual diagnosis treatment centre — one that handles both simultaneously. When the system stays fragmented, so does recovery.
The Need for Integrated Treatment
Actual dual diagnosis treatment involves more than just giving antidepressants in rehab. It requires a coordinated plan — psychiatric evaluation, detox support, medication (if necessary), therapy, and aftercare. Evidence-based approaches like CBT and DBT can help address the core beliefs and coping deficits underlying both disorders.
The ;ld standard? A centre that understands trauma, addiction, medication, attachment wounds, and how all of them intersect. Centres like Samarpan, one of Asia’s leading integrated mental health and addiction facilities, are shaping the future of what dual diagnosis addiction treatment can and should look like.
Why Undiagnosed Dual Diagnosis Is Dangerous
When one condition is treated and the other ignored, relapse is likely. You can remove the substance, but if the depression remains, you’ve just stripped someone of their coping tool without giving them anything new.
Worse, untreated mental illness can escalate. Anxiety can morph into panic. Depression can deepen into suicidality. And each relapse chips away at the individual’s belief that recovery is possible.
That’s not just poor treatment. That’s a systemic failure.
A Better Way Forward
We need clinicians who ask the right questions, even the uncomfortable ones.
We need centres that don’t treat addiction like a moral failing and mental illness like an afterthought.
We need models of care where people are seen, not separated into boxes.
We need language that helps people say, “I’m not just an addict. I’m someone in pain who also struggles with my mind.”
Because that’s how healing starts — not just with detox, but with recognition.
Frequently Asked Questions
How do you deal with a dual diagnosis?
Through integrated care that addresses both the mental health disorder and the addiction. This often includes therapy (like CBT and DBT), medication management, group support, and relapse prevention.
What are the benefits of dual diagnosis treatment?
It reduces relapse risk, improves long-term mental health, and helps people feel understood rather than pathologised. It treats the whole person, not just the symptoms.
What is the new name for dual diagnosis?
The term "co-occurring disorders" is increasingly used in clinical settings, highlighting the interconnected nature of these conditions.
What is the best example of a dual diagnosis?
Common examples include alcohol use disorder with depression, or cocaine addiction with bipolar disorder. These combinations are more common than people realise.
How can Samarpan help?
At Samarpan Recovery Centre, Asia’s leading dual diagnosis treatment center and drug rehabilitation facility, we understand the layered complexity of dual diagnosis, the coexistence of a mental health condition alongside substance abuse. Unlike standard rehab approaches that focus only on addiction, dual diagnosis treatment requires an integrated, nuanced model. Individuals struggling with alcohol withdrawal, substance withdrawal symptoms, or drug use often suffer from underlying personality disorders, depression symptoms, anxiety symptoms, or trauma&mdashgoingl of which may be overlooked without the right care. Many times, the causes of substance abuse are deeply rooted in unresolved emotional pain or undiagnosed psychiatric conditions, which is why dual diagnosis addiction treatment is essential. At Samarpan, our clinical team excels in identifying these overlapping patterns, using expert psychiatric evaluations, evidence-based therapy, and trauma-informed interventions. As one of the most advanced dual diagnosis rehab facilities in Asia, we don’t separate the mind from the substance we treat them together. Our compassionate and holistic model, supported by robust mental health awareness, ensures each client receives tailored care within our world-class dual diagnosis treatment centers, offering not just relief but a sustainable path toward lasting recovery.


















 Yes, many offer serene environments and solid therapeutic frameworks. However, quality varies, so it’s essential to research accreditation, staff credentials, and therapeutic depth.
Yes, many offer serene environments and solid therapeutic frameworks. However, quality varies, so it’s essential to research accreditation, staff credentials, and therapeutic depth.




