Amphetamine-type stimulants don’t sit neatly in one category. They aren’t one drug, one scene, or one kind of user. ATS includes substances that are prescribed, diverted, synthesised, rebranded, and circulated across vastly different social settings , from clubs to classrooms, factories to exam halls.
What links them isn’t culture. It’s effect.
Amphetamine-type stimulants are designed to push the nervous system beyond its natural limits. They increase alertness, confidence, endurance, and emotional detachment. In the short term, they feel productive. In the long term, they extract a cost that often shows up slowly, behaviourally, and psychologically , long before it becomes medically obvious.
Understanding the characteristics of ATS use matters because stimulant addiction rarely looks like “collapse” at first. It looks like performance.
What Counts as ATS and Why Use Has Expanded
ATS includes substances such as amphetamine, methamphetamine, MDMA (ecstasy), and a growing range of synthetic stimulants. Some are prescribed legally in controlled settings. Many are diverted or produced illicitly. All act on similar neurochemical pathways.
The growth in ATS global use is driven by three overlapping factors: availability, perceived utility, and cultural reward systems. Stimulants help people stay awake, work longer, suppress appetite, and feel socially confident. In societies that value output and endurance, that effect becomes attractive.
This is why synthetic stimulant abuse has expanded across regions with very different legal systems and cultural norms. The demand is not niche. It’s structural.
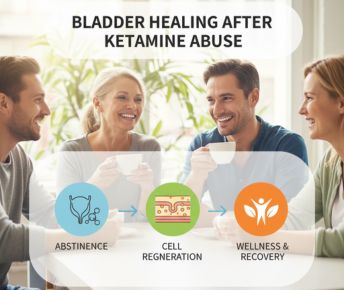
Recognising Common Patterns of ATS Use
One of the defining ATS use patterns is escalation without awareness. People don’t usually start using amphetamines to get high. They start to get through something: deadlines, shifts, exams, social anxiety, emotional exhaustion.
Typical patterns include increasing frequency, shortening gaps between use, and expanding reasons for use. What begins as occasional becomes situational, then habitual.
This is where ats drug abuse develops , not through loss of control at first, but through reliance.
Methamphetamine vs Amphetamine
Understanding methamphetamine vs amphetamine is important clinically. While both are stimulants, methamphetamine crosses the blood–brain barrier more efficiently and produces a stronger, longer-lasting dopamine surge.
This makes meth more reinforcing and more neurotoxic over time. Amphetamine dependence can develop gradually. Methamphetamine dependence tends to form faster and carry higher risks of psychiatric complications.
That distinction matters when assessing severity, treatment needs, and relapse risk.
Behavioural Changes That Appear With Regular Use
The most visible characteristics of ATS use are behavioural rather than physical. People often become more talkative, restless, driven, or irritable. Sleep is delayed. Meals are skipped. Social behaviour becomes either hyper-engaged or unusually detached.
Over time, stimulant addiction symptoms include impulsivity, reduced frustration tolerance, paranoia, emotional flattening, and difficulty stopping once started. Productivity may initially increase, then collapse as burnout and dysregulation set in.
Friends often notice personality changes before users do.
Effects on Sleep, Appetite, and Mood
Few drug classes disrupt basic biological rhythms as profoundly as stimulants. Amphetamine effects on brain circuits responsible for sleep and appetite regulation are significant.
Sleep becomes fragmented or absent. Appetite suppression leads to weight loss and nutritional deficiencies. Mood fluctuates sharply , confidence during use, irritability and low mood afterward.
Over time, this cycle destabilises emotional regulation. Anxiety and depression become more pronounced, particularly between doses. This is often mistaken as a reason to keep using rather than a consequence of use.
Youth and Early Exposure
Youth stimulant abuse is a growing concern globally. ATS substances are often perceived as “study aids,” party drugs, or focus enhancers. Early exposure increases the risk of dependence and long-term cognitive effects because the brain is still developing.
Young users are particularly vulnerable to believing they are in control because consequences are delayed. By the time problems appear, patterns are already entrenched.
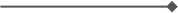
Overdose and Medical Risk
Stimulant overdose signs differ from opioid overdoses and are sometimes missed. They include extreme agitation, overheating, chest pain, irregular heartbeat, seizures, confusion, or collapse.
Repeated high-dose use increases cardiovascular risk, stroke risk, and the likelihood of psychosis. These risks rise sharply when stimulants are combined with alcohol, benzodiazepines, or other psychoactive substances.
Long-Term Health and Cognitive Impact
Long-term amphetamine dependence is associated with memory impairment, reduced attention, emotional dysregulation, and changes in brain reward pathways. Chronic use can also affect cardiovascular health, dental health, and immune function.
In cases involving methamphetamine, the risk of lasting cognitive and psychiatric impairment is higher. This is why long-term ats drug abuse is increasingly recognised as both a neurological and mental health issue.
The Role of Illegal Markets
The illegal stimulant trade has expanded rapidly due to low production costs and high demand. Illicit ATS often vary widely in purity and potency, increasing overdose and toxicity risk.
Unregulated supply also means users often don’t know what they’re taking. This unpredictability is a major driver of harm.
When Someone May Need Help
Signs that someone may need support for ATS dependence include inability to sleep without stimulants, anxiety or depression between uses, increasing tolerance, loss of control over use, paranoia, or neglect of basic needs.
Withdrawal from stimulants is often psychological rather than physically dangerous, but it can be intense. Low mood, exhaustion, anhedonia, and cravings make relapse common without structured support.
Why ATS Use Requires a Different Conversation
ATS are often misunderstood because they initially appear functional. They don’t sedate. They don’t slow. They enhance , until they don’t.
The danger of psychoactive stimulants lies in how convincingly they mimic competence before dismantling it. Treating ATS use as a moral issue misses the point. Treating it as a health and systems issue opens the door to effective intervention.
FAQs
How can you recognise typical patterns of amphetamine-type stimulant use?
Escalating frequency, using for productivity or coping, reduced sleep, appetite suppression, and increasing reliance to function.
What behavioural changes do people usually show when using ATS regularly?
Restlessness, irritability, impulsivity, emotional flattening, paranoia, and changes in social engagement.
How does ATS use affect sleep, appetite, and mood over time?
It disrupts circadian rhythms, suppresses appetite, and creates mood instability, often worsening anxiety and depression between doses.
What health risks are linked to long-term ATS or methamphetamine abuse?
Cardiovascular damage, cognitive impairment, psychiatric symptoms, overdose risk, and dependence.
What signs suggest someone may need help for ATS dependence or withdrawal?
Loss of control over use, sleep deprivation, emotional instability, paranoia, and difficulty functioning without stimulants.
How can Samarpan help?
At Samarpan Recovery Centre, we frequently notice individuals struggling with amphetamine-type stimulant (ATS) use, a pattern that often looks very different from other substance dependencies and is therefore easy to miss or minimise. ATS use is commonly marked by bursts of extreme energy, heightened confidence, reduced need for sleep, appetite suppression, intense focus, and a sense of emotional or cognitive “sharpness” that feels productive at first. Over time, however, these highs are followed by severe crashes, irritability, paranoia, anxiety, emotional flatness, and profound exhaustion. Many people using ATS also experience compulsive behaviours, social withdrawal, aggression, risky decision-making, and a growing inability to function without the drug. At Samarpan, we understand that ATS use is rarely just about stimulation; it is often tied to performance pressure, unresolved trauma, emotional dysregulation, or the need to escape inner emptiness. Our treatment approach combines medical stabilisation with deep therapeutic work using CBT, DBT, and trauma-focused therapy to help clients manage cravings, rebuild sleep and emotional regulation, and address the psychological drivers behind stimulant use. Removed from high-risk environments and supported by a structured, compassionate setting, clients are given the space to slow down, reconnect with their bodies, and recover sustainably. As one of Asia’s leading rehabilitation centres, Samarpan treats ATS use not as a character flaw, but as a signal that the nervous system needs care, containment, and long-term healing.




















 Yes, many offer serene environments and solid therapeutic frameworks. However, quality varies, so it’s essential to research accreditation, staff credentials, and therapeutic depth.
Yes, many offer serene environments and solid therapeutic frameworks. However, quality varies, so it’s essential to research accreditation, staff credentials, and therapeutic depth.




