Borderline personality disorder (BPD) is a challenging mental health illness marked by profound instability in mood, interpersonal interactions, self-image, and self-harming demeaner that can harm themselves and others. Some people use alcohol or drugs to cope with the symptoms of a mental health problem, while others develop substance addiction as a result of inordinate use and must deal with a dual diagnosis.
Impulsivity and Substance Abuse:
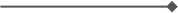
Individuals with BPD frequently battle with impulsivity, which disrupts many parts of their lives. This temerarious behavior and recklessness contributes substantially to the risk of substance dependence. Individuals with BPD may engage in dangerous behaviors, such as drug or alcohol experimentation, as a way to cope with overwhelming and all kinds of inundating emotions due to their impulsive nature. Impetuous Behavior: BPD impulsivity can present itself in a variety of ways, including hazardous driving, excessive and exorbitant food consumption, self-harm, and dependency on substances. Individuals with BPD frequently experience intense and rapidly altering emotions. Impulsive behavior can be a coping mechanism for dealing with overwhelming emotional situations.
BPD is linked to issues managing impulses. This lack of control can lead to impulsive and potentially hazardous behavior, such as misuse of drugs.
Substance Abuse in BPD:
High Prevalence: Studies consistently reveal that individuals with BPD have a high prevalence of substance use disorders. The co-occurrence of several disorders can make diagnosis and treatment more difficult.
Self-Medication: Some people with BPD may self-medicate with substances to relieve emotional pain or suffering. Substance abuse may be a coping mechanism for the high emotions linked with BPD.
Impaired Decision-Making: In BPD, impulsivity and poor impulse control can lead to impaired decision-making, making people more likely to engage in substance abuse without fully contemplating the implications.
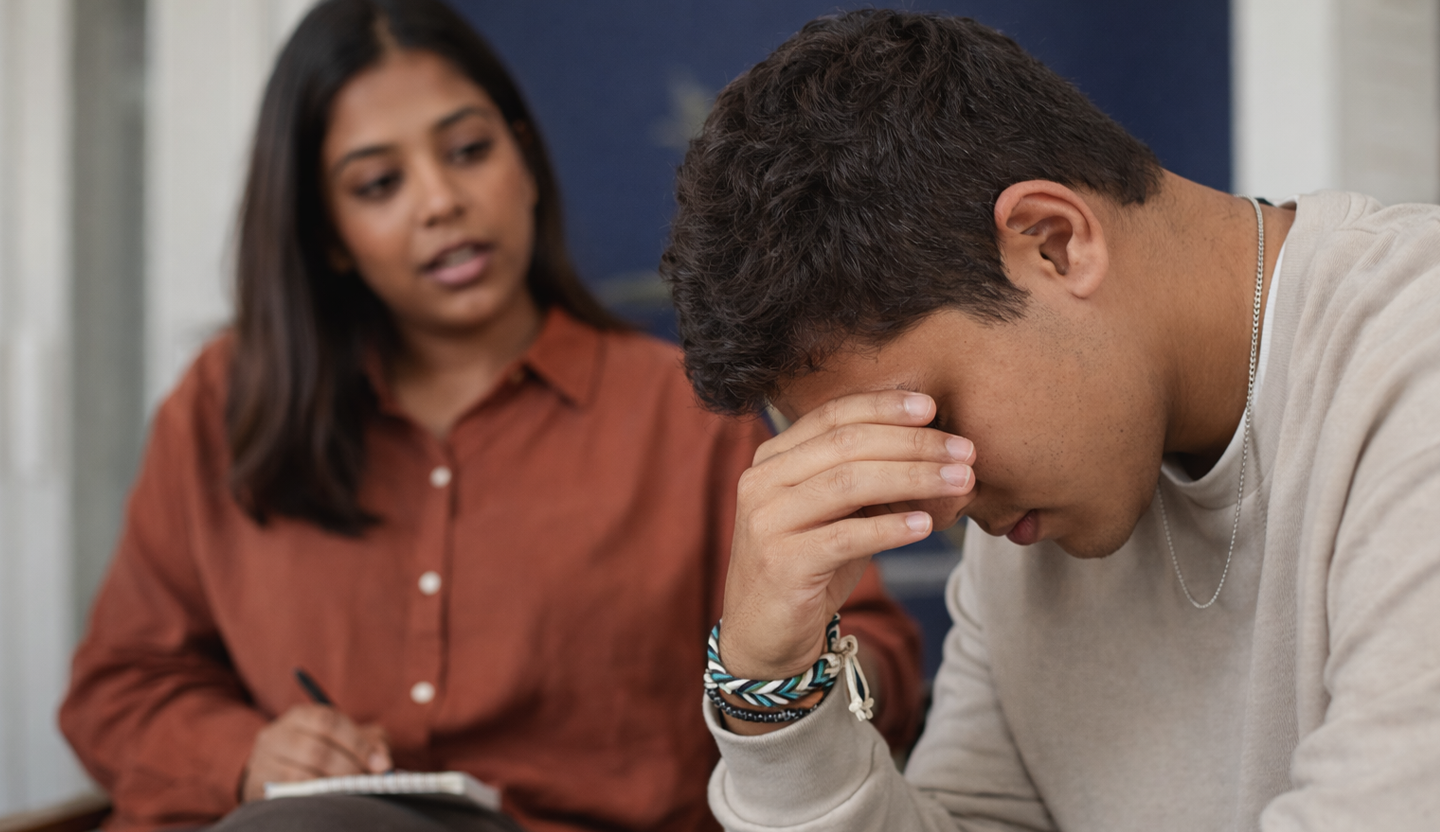
Biochemical Aspects: Brain Circuitry: Studies denote that people with BPD may have transmutations in the brain circuitry that ;vern impulse control. Impulsive behaviors may be caused by dysfunction in regions such as the prefrontal cortex, which is involved in impulse control and decision-making.
Neurotransmitters: Substance use disorders and Borderline Personality Disorder are linked to dysregulation of neurotransmitters including dopamine and serotonin. These abnormalities could be a factor in impulsive actions and an incremental risk of substance dependence.
Among those with BPD, a consequential rate of traumatic childhood experiences is present. Sexual abuse is one of the most prevalent types of abuse, along with abuse and neglect, which are some of the main childhood traumas reported by victims. Supplementally, caregiver loss are prevalent in the early years of BPD patients, according to research. Adults with borderline personality disorder (BPD) frequently report that the people who raised them did not give them the opportune aegis and frequently queried the sincerity of their emotions. It has been determined that caregivers who exhibit erratic conduct and emotional disengagement are frequently BPD or impulsive subtype persons. Disrupted estrogen levels have been connected to BPD. These kinds of estrogen levels are sometimes experienced by women during their menstrual cycle. People with endometriosis are not the first to get hormone-cognate treatment, and ri;rous PMS is handled differently from borderline personality disorder (BPD) There have been numerous reports of brain abnormalities linked to borderline personality disorder (BPD). Among these include amygdala and hippocampal atrophy. People with BPD usually have less activity in their prefrontal cortex than people without the disorder. Cortisol is produced by the hypothalamic-pituitary-adrenal axis, and it is usually elevated in BPD patients. Sufferers who already have high calibers of cortisol production may experience experiences as traumatic. On the other hand, stressful childhood experiences might cause cortisol production, which could lead to an excess of cortisol being produced. The aim of BPD causal research is heritability. A study conducted in the Netherlands discovered that chromosome nine is associated with BPD traits and that genetic influence accounted for 42% of the diversity in features across sufferers. Other genes that are now being studied for their potential role in the development of BPD include DAT, which has been linked to problems in inhibitory regulation, and DRD4, which has also been linked to disordered attachment. Researchers are also investigating additional potential risk factors for BPD development. Certain elements, such as social and familial stability, are being investigated and may prove to be important in the development of borderline personality disorder (BPD). This disorder can be prevented from developing in a stable family environment.
Emotional Dysregulation and Coping Mechanisms: Emotional dysregulation is a hallmark of BPD, with individuals experiencing intense and rapidly shifting emotions. The use of substances can serve as a maladaptive coping mechanism, providing temporary relief from emotional distress. Substance abuse may be a misguided attempt to self-medicate and alleviate the overwhelming emotional pain associated with BPD.
Identity Issues and Escapism: A sedulously erratic sense of self is one of the hallmarks of borderline personality disorder. Since their concept of self lacks a distinct and definable core, the question of personal identity is nebulous. They are an amassment of conceptions, feelings, predilections, prospects, and experiences. The conception of a personal identity is dynamic and ever-evolving since these things are perpetually being integrated to and modified. What does having a sense of self entail? To feel a sense of self is, in general, to have an internal point of reference that is bulwarked and shielded from transmutations in the outside environment, albeit a precise description is hard to come by. This is not to argue that their sense of self is impervious to events in their environment, but rather that the fundamental elements of their identities do not alter just because their external circumstances changes. Even if you experience a personal loss, a breakup, or lose your job, you can still be a feline person! Those who have BPD frequently find that this is not the case.To be pellucid, identity crises are not exclusive to those with BPD. Everybody will ineluctably experience ups and downs in life, and at some point they will commence to doubt their identity, credences, and actions.
This is typical. Identity crises of the kind associated with BPD are mundane. Depending on the person they are with, a person with BPD will frequently alter their comportments, predilections, looks, and mannerisms. This explicates why they may infrequently be called "chameleons," as they alter their skin to coalesce in with their environment. BPD patients may turn to outside sources, such as substance abuse, in an endeavor to find a sense of identity because of the disorder's unstable self-image. Alcohol and drug use might provide a brief reprieve from the perpetual identity confusion and vacuousness that BPD sufferers endure.
Interpersonal Difficulties and Isolation:
Because of their interpersonal issues and trepidation of abandonment, people with BPD frequently find it arduous to establish and maintain solid relationships. These difficulties can be made worse by substance misuse, which can cause isolation as relationships break down due to addiction-related behaviours. Substance misuse cycles have the potential to further distance addicts from the avail they much require.
Self-Harm and the Intersection with Substance Abuse:
Substance misuse can be linked to self-harming deportments, which are frequently linked to BPD. People may self-medicate with drugs to facilitate their emotional distress or they may participate in hazardous activities that imperil their health. When designing a treatment program, the connection between substance misuse and self-harm must be conscientiously considered.
How can Samarpan help you?
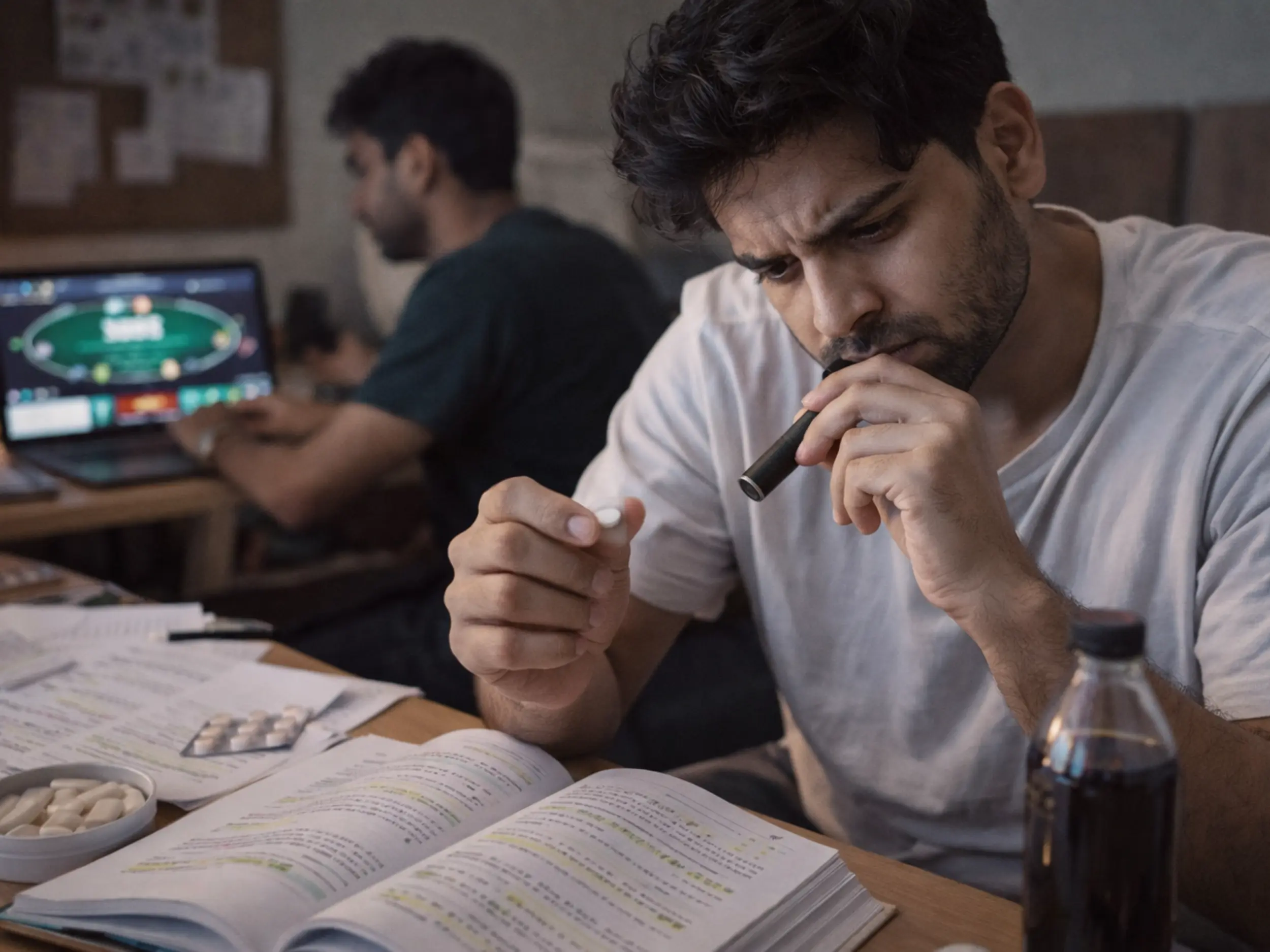
Samarpan uses Evidence-predicated psychotherapy and offers people with BPD the chance to examine their feelings, conceptions, and actions in a secure and emboldening setting. Many strategies, such as Dialectical Deportment Therapy (DBT), Cognitive Behavioral Therapy (CBT), and Schema-Focused Therapy, have demonstrated efficacy in treating the symptoms of Borderline Personality Disorder (BPD).
Treatment Challenges and Dual Diagnosis:
Treatment for BPD and drug use disorders that co-occur presents particular difficulties. An integrated strategy is indispensable because the recovery process may become more arduous due to the intricacy of BPD symptoms. Dialectical Behaviour Therapy (DBT), a therapeutic modality that places an accentuation on adeptness development and emotional regulation, has demonstrated efficacy in treating both BPD and addiction.
Evidence-predicated psychotherapy, which is a key component of BPD treatment, is utilized by Samarpan. It offers people with BPD the chance to examine their feelings, conceptions, and actions in a secure and emboldening setting. Many strategies, such as Dialectical Deportment Therapy (DBT), Cognitive Behavioral Therapy (CBT), and Schema-Focused Therapy, have demonstrated efficacy in treating the symptoms of Borderline Personality Disorder (BPD).
Developing prosperous interventions requires a construal of the interactions between identity challenges, emotional dysregulation, impulsivity, and interpersonal difficulties. People can commence along a road to recuperation that takes into account the intricacy of their phrenic health and addiction concerns by treating both the underlying quandaries linked to BPD and the difficulties associated with substance usage.
Samarpan is a specialized international Substance Use Disorder (De-Addiction) and Process Addiction rehab in Pune, India that accepts a maximum of 26 clients. We only accept clients on a voluntary basis and have a highly structured program that encompasses the most effective approaches to Substance Use Disorder and addiction. The facility is set in the rolling hills Mulshi, with clients having either individual or shared rooms, in a modern resort-like facility, staffed by Internationally Accredited Professionals. Samarpan is fully licensed under The MSMHA and is also an accredited ;RSKI-CENAPS Centre of Excellence offering a program from 5 to 13 weeks.
If you or someone you care about is considering treatment for substance use disorder or process addictions, we can help. Contact us now on admissions@samarpan.in or phone/WhatsApp us on +91 81809 19090.