Myriad young people with substance abuse disorders and depression commit suicide. One consequential risk factor for suicide endeavors is substance abuse. Suicide rates are significantly higher among those who struggle with addiction than in the general population. Twenty percent of suicide deaths contain opioids, while proximately a quarter of suicides involve alcohol consumption. A plethora of people with mood disorders turn to drugs and alcohol as a kind of self-medication to get through arduous times. Exorbitant consumption of alcohol and drugs can develop into a substance use disorder, which can exacerbate depressive episodes and raise the jeopardy of suicide.
Using Drugs to Get Over Pain:
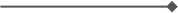
When people feel helpless, they will prehend for everything material in an endeavor to "escape" or abate their a;ny. These defenseless moments—Fight, Flight, Freeze—can expeditiously lead to overindulgence in pabulum, drink, nicotine, narcotics, sex, employment, and reading. Lamentably, some "survival mechanisms" or "coping skills" are more deleterious to the body or the "family," and they certainly magnetize more shame or censure.
Never should we judge someone else for the coping strategy they have opted for. Kenning "escape" or "flight" mode makes it more facile to realize that drug use and other coping techniques are genuinely surface-level replications to underlying quandaries.
Substance abuse is a prevalent coping mechanism utilized by people who are experiencing emotional anguish, trauma, or phrenic health quandaries to dull their feelings.
The short elude that substance use might initially offer can lead to a vicious cycle where people become dependent on drugs to evade dealing with underlying phrenic anguish.
You will additionally commence to see that inordinate corpulence is an big quandary in our culture that claims lives and lowers self-esteem, even though food addictions can be simpler to surmount in society than drug addictions.
Neurological factors:
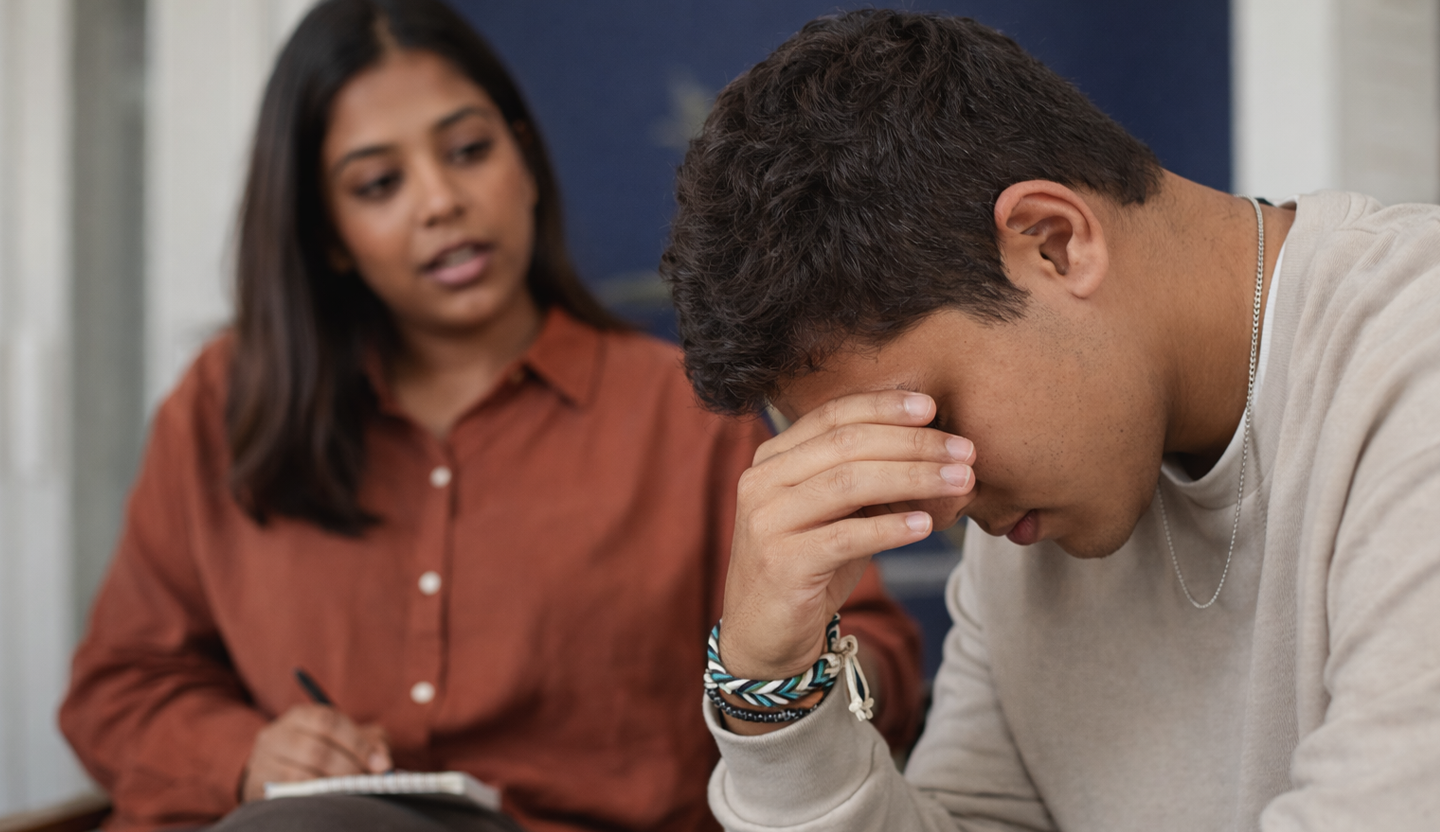
Substance abuse's effects on brain chemistry might worsen thoughts. Vicissitudes in neurotransmitter levels brought on by drugs may disrupt mood control, the overall mental health hence incrementing the likelihood of depression and suicide thoughts. Substance abuse can cause certain neurotransmitter pathways to be overstimulated or inhibited, leading to imbalances that have a consequential impact on mental health.
Addiction and the brain's reward system are proximately close. This system is stimulated by several addictive substances, which raise dopamine levels, engender a euphoric feeling, and enhearten substance utilization. Perpetual substance use can ineluctably desensitize the encephalon's reward pathways, requiring more preponderant doses of the drug to have the same delectable effect. This desensitization is linked to anhedonia, which is a diminished capacity for bliss that is frequently seen in addiction and despair.
Long-term substance addiction can alter the structure of the brain, especially in areas cognate to impulse control, decision-making, and emotional regulation. Transmutations in the prefrontal cortex, which controls executive skills, and the amygdala, which processes emotions, might impact a person's capacity to control stress and emotional reactions. Susceptibility to mental health conditions like depression and suicide phrenic conceptions is exacerbated by these vicissitudes.
Solicitousness, dejection, and irritability are among the mental health symptoms that substance withdrawal frequently causes. Withdrawal discomfort might aggravate mental health conditions that already subsist or accommodate as a catalyst for suicide cerebrations. People may struggle to find coping strategies for their mental distress, which victuals the cycle of substance abuse as a kind of self-medication.
Addiction and mental health conditions may be impacted by epigenetic modifications, which are variations in gene expression without alterations to the underlying DNA sequence. Epigenetic changes brought on by environmental variables, such as substance abuse, can heighten vulnerability to mental health issues. These alterations endure and impact a person's reaction to stress, possibly playing a role in the co-occurrence of addiction and suicide ideation. Comprehending these biological elements emphasizes the importance of adopting a comprehensive therapeutic strategy. Treatments that target the underlying neurobiological mechanisms of addiction and mental health issues can promote recovery and reduce the likelihood of relapse. Dual-diagnosis programs that combine therapeutic and pharmaceutical interventions are specifically designed to address these complex biological relationships, providing a thorough and efficient route to recovery.
What are the Underlying Elements?
Kindred risk factors, such as a history of trauma, abuse, or a propensity for mental health illnesses, can give ascend to both addiction and suicidal ideation.
Addiction and suicidal cerebrations can arise as a result of both environmental factors and genetic predispositions.
These are the common factors!
Similar risk factors, such as a history of trauma, abuse, or a propensity for mental health illnesses, can give ascend to both addiction and suicidal ideation.
Addiction and suicidal thoughts can arise as a result of both environmental factors and genetic predispositions.
Social shame and isolation are commonplace for people struggling with addiction and suicide thoughts, which exacerbates their emotional difficulties. This common experience of marginalization can strengthen the connection between these two difficulties.
Things like losing your work, having quandaries in your relationships, or having licit concerns might accommodate as triggers, escalating your mental pain and rekindling your thoughts of suicide.
An unhealthy exacerbation of the two problems may result from people turning to drugs more frequently in an attempt to self-medicate in order to soothe their emotional suffering.
Methods of Therapy:
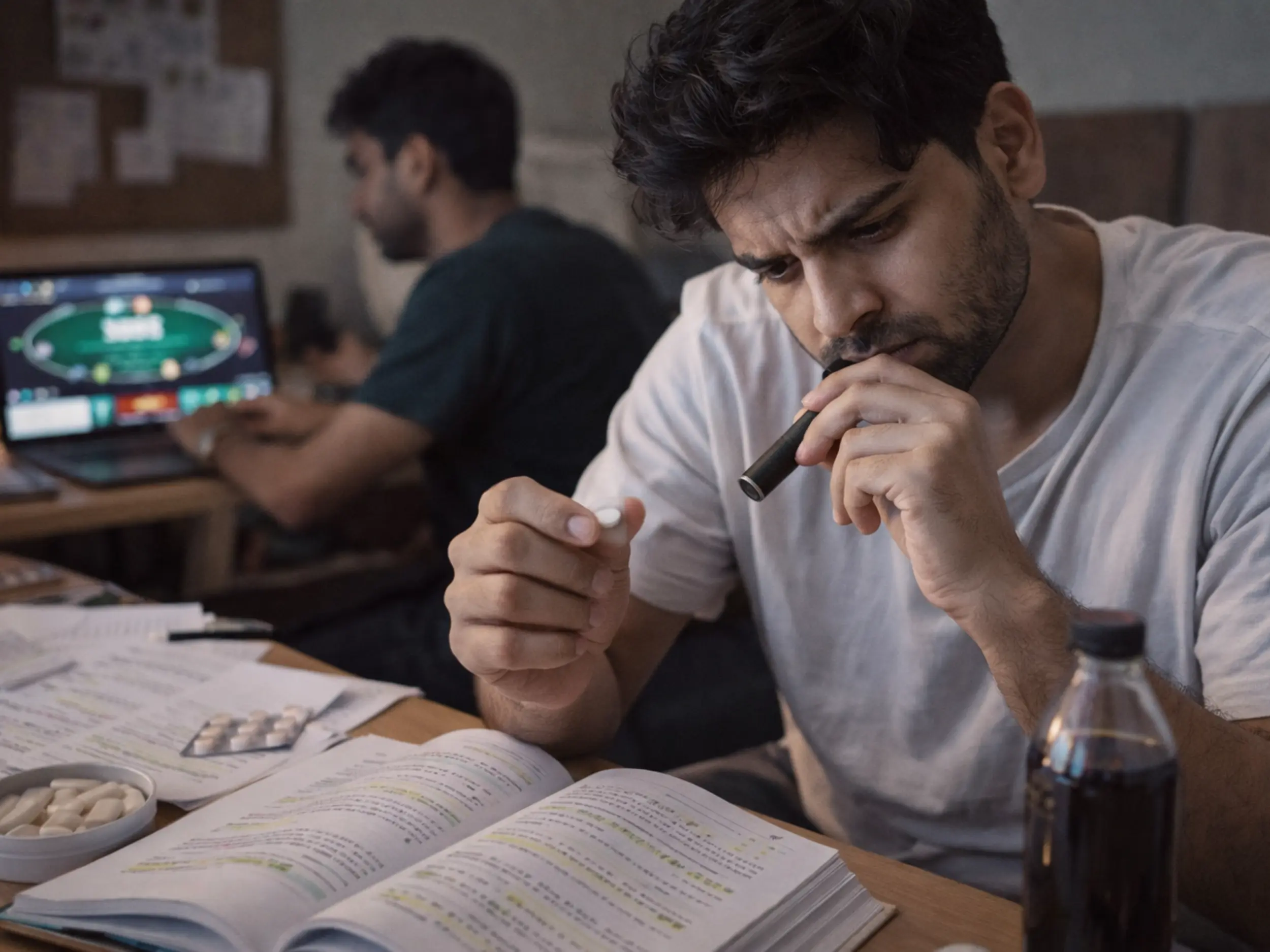
Comprehensive treatment strategies addressing both addiction and mental health concerns are crucial for breaking the cycle. Dual-diagnosis programs that integrate therapy, counseling, and pharmacological interventions can be efficacious.
Therapies including dialectical behavior therapy (DBT) and cognitive-behavioral therapy (CBT) have demonstrated promise in treating addiction and suicidal ideation.
Similar to 12-step organizations, mutual assistance groups offer a caring environment where people can tell their stories and work toward recovery.
In order to empower people to seek treatment without fear of rejection, it is imperative that efforts be made to lessen the stigma that society attaches to addiction and mental illness.
How can Samarpan help?
Samarpan approaches this with CBT which strengthens resistance against suicide thoughts and allows people to handle pressures without turning to drugs. It does this by focusing on maladaptive thought patterns and actions. Through DBT, it promotes emotional control by combining acceptance and mindfulness, which lessens the need for drugs as a coping strategy and lowers the likelihood of suicidal thoughts.
It is possible to provide those coping with these challenging situations hope and support by endorsing integrated treatment approaches and severing the loop of hopelessness. Fostering open communication, reducing stigma, and creating a sense of community are essential to severing the link between addiction and suicidal thoughts and to fully healing and recovering.
Samarpan is a specialized international Substance Use Disorder (De-Addiction) and Process Addiction rehab in Pune, India that accepts a maximum of 26 clients. We only accept clients on a voluntary basis and have a highly structured program that encompasses the most effective approaches to Substance Use Disorder and addiction. The facility is set in the rolling hills Mulshi, with clients having either individual or shared rooms, in a modern resort-like facility, staffed by Internationally Accredited Professionals. Samarpan is fully licensed under The MSMHA and is also an accredited ;RSKI-CENAPS Centre of Excellence offering a program from 5 to 13 weeks.
If you or someone you care about is considering treatment for substance use disorder or process addictions, we can help. Contact us now on admissions@samarpan.in or phone/WhatsApp us on +91 81809 19090.